Duke Heart Network partners with hospitals to reduce contrast-induced acute kidney injury (AKI) in patients. By working hand-in-hand within hospital teams, Duke provides real-time monitoring, multidisciplinary collaboration, and sustainable strategies that enhance patient safety, improve quality metrics, and optimize healthcare efficiency.
At Duke Heart Network, we know that real progress in patient care comes from collaboration. That’s why we work alongside hospitals and healthcare institutions to implement data-driven improvement strategies that optimize outcomes, reduce costs, and enhance patient safety.
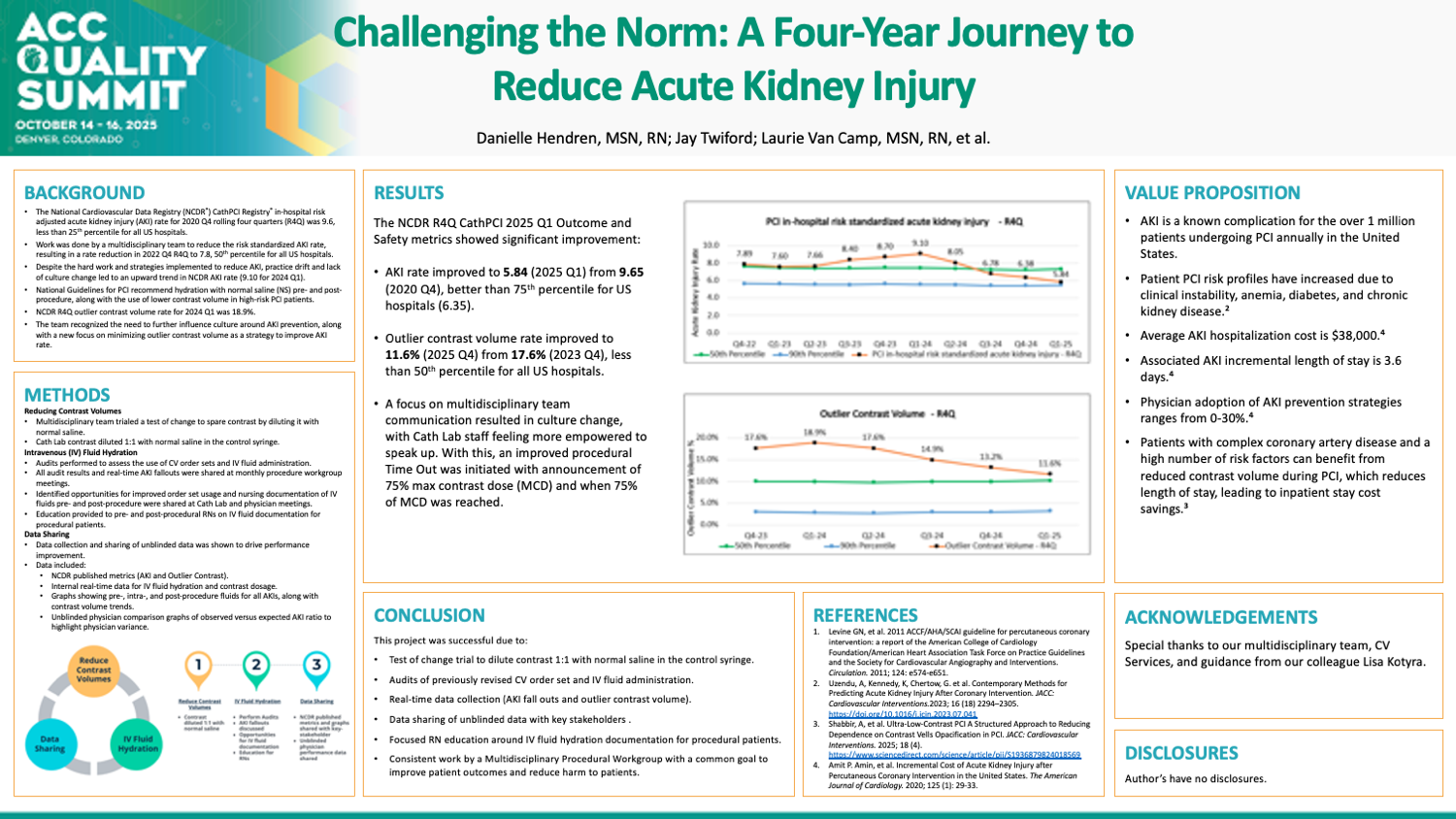
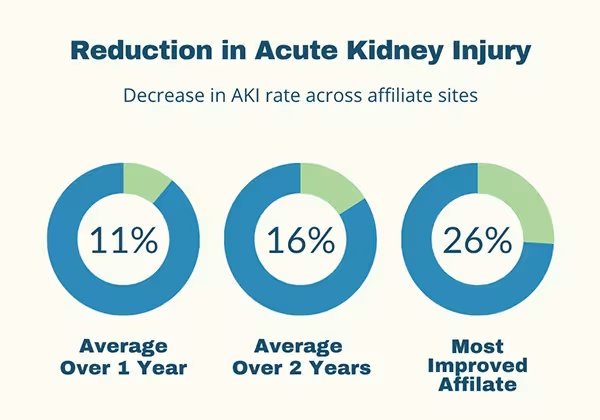
One of the most critical challenges we help hospitals address is reducing contrast-induced acute kidney injury (AKI) in percutaneous coronary intervention (PCI) patients. By refining prevention strategies, hospitals not only improve patient safety but also strengthen performance in national benchmarks such as the National Cardiovascular Data Registry (NCDR®) CathPCI Registry®.
Why AKI prevention matters
AKI prevention isn’t just about improving clinical outcomes—it’s about making a real difference in patient care while reducing the financial strain on healthcare systems. The data speaks for itself:
- Hospitalization costs for AKI patients nearly double, averaging $38,869 compared to $17,1671
- AKI extends hospital stays by an average of 3.6 days, adding resource burdens¹
- The estimated U.S. healthcare cost burden exceeds $1.67 billion annually²
- Hospitals participating in CMS’s Bundled Payments for Care Improvement Advanced model can significantly improve cost efficiency through AKI reduction strategies
- The 50th percentile AKI rate for PCI patients is 7.3%, leading to increased complications³
With so much at stake, the need for a structured, multidisciplinary approach to AKI prevention has never been more critical.
The Duke Heart Network approach
At Duke Heart Network, we don’t just provide recommendations—we embed ourselves within hospital teams to create sustainable, long-term improvements. Our process includes:
- A Comprehensive Cath Lab Assessment – We evaluate hydration protocols, pre-procedure lab testing, and contrast administration strategies to identify improvement opportunities.
- Multidisciplinary Collaboration – Bringing together physicians, nurses, and quality improvement specialists, we develop targeted intervention strategies using real-time data analysis.
- Real-Time Monitoring and Benchmarking – Key metrics such as contrast use, left ventriculogram rates, and hydration compliance are tracked to measure success.
- Physician and Nursing Leadership Engagement – We identify champions within the hospital to drive best-practice adoption and long-term sustainability.
- Transparency and Accountability – Unblinded provider comparisons encourage a culture of continuous quality improvement.
- Recognition and Impact – We collaborate with hospitals to submit project abstracts to quality conferences, highlighting their commitment to patient care excellence.
A partnership that delivers results
By taking a hands-on, data-driven approach, Duke Heart Network empowers hospitals to reduce AKI complications, improve quality metrics, and enhance financial performance. When healthcare institutions partner with us, they gain access to a team of experts, proven methodologies, and the tools necessary to create lasting, meaningful change. AKI prevention is more than an initiative—it’s an investment in better patient outcomes and a stronger healthcare system.
References:
- Amin, A.P., et al. (2020). Incremental Cost of Acute Kidney Injury After Percutaneous Coronary Intervention in the United States. The American Journal of Cardiology, 125(1), 29-33
- Prasad, A., et al. (2020). Contemporary Trend of Acute Kidney Injury Incidence and Incremental Cost Among U.S. Patients Undergoing Percutaneous Coronary Procedures. Catheterization and Cardiovascular Interventions, 96(6), 1184-1197
- National Cardiovascular Data Registry (NCDR®) CathPCI Registry® – Contrast-induced acute kidney injury (AKI) rates and benchmarking data